Research article/ Open Access
DOI: 10.31488 /bjhd.118
Long- Term Outcomes Following Endocardial and Epicardial Ablation of Atrial Fibrillation in a Low Procedural Volume Hospital
Kim M. Williams, MPH*, Patrick J. Blatchford, PhD, Frank A. Laws, MD FACC
Valley View Hospital, 1906 Blake Ave, Glenwood Springs, CO USA
*Corresponding author: Kim M. Williams, MPH, Valley View Hospital 1906 Blake Ave, Glenwood Springs, CO 81601 USA, Tel: 01 970-384-7433; (f) 01 970-384-8024.
Abstract
Atrial Fibrillation (AFib) ablation volume and its relation to outcomes posit negatively for low volume centers, the ideal annual hospital volume is 50. Fifty four in-patients have been followed. The primary outcome is the change in an AFib validated outcomes questionnaire that subjects completed pre-procedure, 6 months, 1 year, and annually thereafter. Secondary endpoints included duration of maintaining normal sinus rhythm (NSR) and adverse events. At 6 months, the overall questionnaire score improved by 30 points from the baseline score (95% CI: (16, 43), p < 0.001). The improvement from baseline was also maintained at 1 year, with the 1-year change score of 22 points (95% CI: (14, 30), p < 0.001), additionally significant improvements were observed in each of the subscales. Based on a Kaplan-Meier analysis, 96% of subjects maintained NSR at 6 months, 87% maintained NSR at 1 year, and 78% maintained NSR at 2 years. Epicardial and endocardial ablation for AF care is feasible in a low-volume ablation hospital with careful long-term tracking. Patients can receive quality care closer to home and not incur costs associated with traveling for health care-a determinate of value- based care.
Introduction
Atrial Fibrillation (AF) is the most common supraventricular arrhythmia presenting in clinical practice, the incidence of AF in the United States is approximately 1.64 million and the prevalence is estimated to reach over 12 million by 2030 [1,2]. The annual AF cost burden to the US health care system is 6 billion and as fiduciaries of value-based health care clinicians are obligated to track outcomes, cost and constantly improve the quality of electrophysiology care delivered. Institute of Medicine (IOM) definition of quality envelopes the utilization of patient –reported outcomes to monitor quality of life and symptom management as an outcome metric [3]. AF downstream sequela is stroke and the treatment goal is prevention of myocardial fibrosis, stoke formation and alleviation of AF symptoms. Catheter ablation and more recently early ablation in the AF disease process has shown to be a more effective treatment option for maintaining normal sinus rhythm compared to medical therapy and improve health-related quality of life [4-6].
Consensus statements suggest facilities perform greater than 50 ablations annually for AF mitigation to improve outcomes for patients [7]. This study aims to report the results the effectiveness of AF ablations from a low volume patient-centered institution with the use of an AF disease specific quality of life questionnaire. Literature posits primary indications for rhythm control are improvement of AF symptoms [8]. Detailed are real-world evidence on the outcomes from a low AF ablation volume hospital.
Methods
This investigator-initiated, all-comers prospective trial is registered with www.clinicaltrials.gov, registration number NCT03428048. The study was approved by the Institutional Review Board (IRB) of ADVARRA IRB, Columbia, MD. USA (Pro00026648) and all interventions were performed in accordance with relevant guidelines and regulations as they specify protection of human subjects’ participation in outcomes research. Informed consent for research was obtained from all subjects prior to enrollment. The primary endpoint is the 6-month change (from baseline which was pre-procedure), in the Atrial Fibrillation Effect on QualiTy-of Life (AFEQT) Questionnaire overall score. The AFEQT is recognized as a validated assessment to clinically follow patients with AF [8]. Secondary endpoints include the 1-year change in AFEQT overall score, the duration of maintaining normal sinus rhythm (NSR), adverse events, and mortality. Maintaining NSR was defined as the length of time (days) until the first recurrence of atrial tachyarrhythmia after reaching 91 days. In alignment with the 2017 expert consensus statement on AF ablations, reoccurrences of atrial tachyarrhythmia during the first 90 days after the index procedure (blanking period) were not counted in the determination of failure of NSR5. The time of maintaining NSR was analyzed using non-parametric Kaplan-Meier survival analysis methods. An adverse event was tracked if it warranted an intervention or resulted in a prolonged length of stay.
Data source
The data was collected prospectively and recorded and stored in a Microsoft Excel workbook. Variables collected included the demographics of age, sex, and race, as well as CHA2DS2-VAS-c, procedural complications and displayed in Table 1. Patient Characteristics.
Study population
From 2017, all patients admitted (no exclusions) for epicardial and endocardial ablation of AF were asked to participate in our outcomes research study, The NEXUS Registry. The patients will be followed for up to ten years after the initial ablation with visits at 6 months and 1-year post-operation and annually thereafter. Patients participate in a shared- decision making process and were asked about their symptoms and function as it relates to AF prior to any ablation procedure.
Post ablation, rhythm status and charts were abstracted to determine if patients required direct current cardioversions (DCCVs) or had an ECG demonstrating AF episodes. Our institution is defined as rural and annually performs < 50 epicardial and endocardial ablations.
Ablation procedures
Most of the patients (57%) received cryoablation followed by the hybrid procedure – a combination of endocardial and epicardial ablation (18%). Ten patients received epicardial ablation – the Modified MAZE (18%) and two patients received laser ablation (3%). The ablation strategy for endocardial ablation is pulmonary vein isolation and was facilitated by one electrophysiologist. Patients that experienced epicardial or surgical ablation (Maze-modified, Hybrid) were under the care of two cardiothoracic surgeons and classified as minimally invasive (non- sternotomy). All patients received general anesthesia, no surgical ablations were preformed concomitantly and hybrid is further defined as endo and epicardial ablation occurring within the same in-patient episode or within three months from the index procedure. Left atrial occlusion is managed with a surgical clip and delineated as such.
Statistical analysis
Subject characteristics of age, sex, CHA2DS2 –VASc score, initial ablation procedure type and serious adverse events through hospitalization were summarized using descriptive statistics, with results presented both overall and by diagnosis type (paroxysmal vs persistent) and shown in Table 1. Continuous numeric variables are summarized using means and extreme values (minimum and maximum), and categorical variables are summarized using frequency counts and percentages. The 6-month and 1-year changes in the overall AFEQT score as well as the 4 subscale scores were tested using a 2-sided paired t-test on the scores at baseline and follow-up (6 months and 1 year), controlling the type 1 error rate at 0.05. The mean change along with the associated 95% confidence intervals (CI) and p-values are presented in Table 2. Outcomes for both the 6-month and 1-year changes along with the baseline mean and standard deviation (SD). The p-values are from the hypothesis test that the scores did not change from baseline. The duration of maintaining NSR was analyzed using a Kaplan-Meier survival analysis and displayed in Figure 1. Normal Sinus Rhythm Duration Post AF Ablation. All analyses were conducted using SAS software, version 9.4 (SAS Institute, Cary, NC, USA).
Table 1:Patient Baseline Characteristics
| Variable | Paroxysmal Diagnosis (N = 36) | Persistent Diagnosis (N = 18) | Total (N = 54) | P-Value | |
|---|---|---|---|---|---|
| Sex | 0.42 | ||||
| Male | N (%) | 22 (61) | 13 (72) | 35 (65) | |
| Female | 14 (39) | 5 (28) | 19 (35) | ||
| Age at Enrollment | 0.74 | ||||
| Years | Mean (SD) | 65.0 (9.4) | 65.9 (9.6) | 65.3 (9.4) | |
| (Min, Max) | (41, 84) | (47, 80) | (41, 84) | ||
| CHA2DS2-VASc Score | 0.49 | ||||
| 0 | N (%) | 5 (14) | 3 (17) | 8 (15) | |
| 1 | 8 (22) | 2 (11) | 10 (19) | ||
| 2 | 9 (25) | 6 (33) | 15 (28) | ||
| 3 | 6 (17) | 5 (28) | 11 (20) | ||
| 4 | 2 (6) | 2 (11) | 4 (7) | ||
| 5 | 5 (14) | 0 (0) | 5 (9) | ||
| 6 | 1 (3) | 0 (0) | 1 (2) | ||
| Initial Ablation Procedure | < 0.001 | ||||
| Cryo | N (%) | 29 (81) | 2 (11) | 31 (57) | |
| Hybrid | 1 (3) | 2 (11) | 3 (6) | ||
| Hybrid/Clip | 0 (0) | 7 (39) | 7 (13) | ||
| Laser | 2 (6) | 0 (0) | 2 (4) | ||
| Maze | 0 (0) | 3 (17) | 3 (6) | ||
| Maze/Clip | 3 (8) | 4 (22) | 7 (13) | ||
| Unknown | 1 (3) | 0 (0) | 1 (2) |
Table 2:Out comes
| Baseline | 6-Month Change | 1-Year Change | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome | Mean (SD) | N | Mean | 95% CI | P-Value | N | Mean | 95% CI | P-Value |
| Overall AFEQT | 59 (25) | 15 | 30 | (16, 43) | < 0.001 | 19 | 22 | (14, 30) | < 0.001 |
| Symptoms Subscale | 64 (28) | 15 | 28 | (14, 41) | < 0.001 | 19 | 19 | (8, 30) | 0.002 |
| Daily Activities Subscale | 58 (31) | 15 | 28 | (10, 46) | 0.005 | 19 | 20 | (11, 29) | < 0.001 |
| Treatment Concerns Subscale | 56 (23) | 15 | 33 | (19, 46) | < 0.001 | 19 | 27 | (18, 37) | < 0.001 |
| Treatment Satisfaction Subscale | 48 (29) | 15 | 48 | (29, 68) | < 0.001 | 19 | 37 | (19, 54) | < 0.001 |
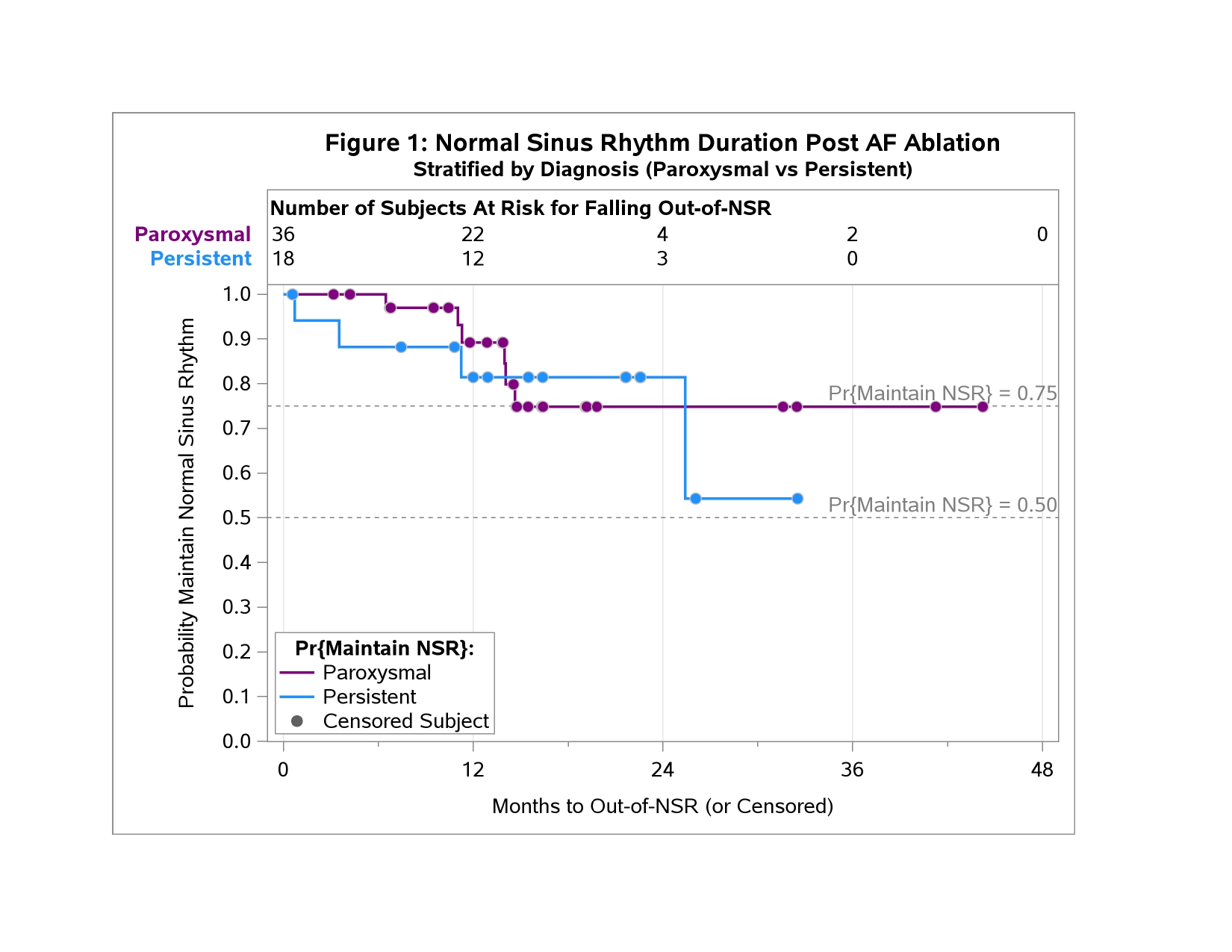
Figure 1:Normal Sinus Rhythm Duration Post AF Ablation Stratified by diagnosis (Paroxysmal vs Persistant). The figure demonstrates results from Kaplan Meir analysis of patients with paroxysmal AF (n=36), the trajectory in the purple line showed that 89% maintained Normal Sinus Rhythm (NSR) at 1 year, and 75% maintained NSR at 2 years, whereas among patients with persistent AF (n= 18), the trajectory in the blue line 81% maintained NSR at both the 1 year and 2 years time points however, at 25 months, patients with persistent AF only 54% maintained NSR.
Results
Between May 2017 and November 2020 54 patients were enrolled into the study and agreed to long-term follow-up. At 6 months post-ablation, the overall AFEQT score increased by a mean of 30 points from the baseline score (95% CI: (16, 43), p < 0.001). The improvement from baseline was also maintained at 1 year, with the overall AFEQT 1-year change score of 22 points (95% CI: (14, 30), p < 0.001). A statistically significant improvement at 6-months (from baseline) was also observed in each of the subscales (symptoms, daily activities, treatment concerns, and treatment satisfaction). Although the 1-year changes were not as great as the 6-month changes, the improvements at 1 year for the overall AFEQT score and all subscales were still statistically significant. Based on a Kaplan-Meier analysis, 96% of subjects maintained NSR at 6 months, 87% maintained NSR at 1 year, and 78% maintained NSR at 2 years as illustrated in Figure 1. When stratified by diagnosis type (paroxysmal versus persistent), Figure 1. demonstrates results from patients with paroxysmal AF, the trajectory in the purple line showed that 89% maintained NSR at 1 year, and 75% maintained NSR at 2 years, whereas among patients with persistent AF, the trajectory in the blue line 81% maintained NSR at both the 1 year and 2 years time points however, at 25 months, patients with persistent AF only 54% maintained NSR . The major complications were pericardial effusion.
Discussion
A retrospective big data study (>90,000 cases) reported low annual operator and hospital volume- defined as <50 ablations/year, was independently associated with complications with an adjusted OR of 1.49 [7]. Furthermore, this analysis illustrated the most frequent adverse outcomes are cardiac complications [7]. Our small prospective study illustrates a low annual operator and hospital volume yields positive results as evidenced by successful management of symptoms and function with an AF disease specific questionnaire with small numbers of complications. A recent meta-analysis of 15 studies demonstrated 72% of patients with paroxysmal AF and hypertrophic cardiomyopathy remained free of AF which is comparable to results from our study 10.
Limitations
Clearly this study is limited by the small sample size and lacks randomization. Outcomes research does not support the level of evidence to pioneer novel AF treatment interventions. The purpose of the study is to demonstrate that low-volume centers and operators can facilitate procedures demonstrated safe and effective from large randomized controlled trials.
Future analyses will include regression analyses to investigate the change in AFEQT scores while controlling for the potential confounding factors of duration of AF diagnosis, number of ablations, and disease staging using hypertrophic cardiomyopathy diagnosis. This will also enable results to be compared with results from previous studies which used a regression framework. This study lacks analysis of qualifying comorbidities and AF staging – other than basic counts in Table1.
Although sinus rhythm is tracked up to 10 years post AF intervention, it is yet to be determined the percentage of patients that remain in NSR over longer periods of time. Long-term follow-up analysis will be continued.
Conclusion
Epicardial and endocardial ablation for AF care is feasible in a low-volume ablation hospital with careful long-term tracking and shared- decision making. Patients can receive quality care closer to home and not incur costs associated with traveling for health care-a determinate of value- based care.
Acknowledgements
None
Declarations of Interest
None
Financial Support
Valley View Hospital
Data Availability
The data underlying this article will be shared de-identified on reasonable request to the corresponding author.
References
1. Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County Minnesota, 1980 to 2000 and implications on the projections for future prevalence. Circulation. 2006; https:// doi.org /10.1161/CIRCULATIONAHA.105.595140.
2. Colilla S, Crow A, Petkun N, et al. Estimates of Current and Future Incidence and Prevalence of Atrial Fibrillation in the U.S. Adult Population. Am J Cardiol. 2013; 112:1142e1147.
3. Institute of Medicine. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press. https://doi.org/10.17226/10027
4. 2019 AHA/ACC/HRS Focused Update of the 2014 Guideline for Management of Patients with Atrial Fibrillation. 10.1016/j.jacc.2019.01.011.
5. 2017 HRS/EHRA/ECAS/APHRS/SOLACE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace. 2018; 20, e1-e160 https://doi.org/10.1093/europace/eux274.
6. Kirchhof P, Camm AJ, Goett A, et al. Early Rhythm- Control Therapy in Patients with Atrial Fibrillation. N Engl J Med. 2020; 383;14.
7. Deshmukh A, Patel NJ, Pant S, et al. In-Hospital complications associated with catheter ablation of atrial fibrillation in the United States between 2000 and 2010: analysis of 93, 801 procedures. Circulation. 2013; 128:2104-2112.
8. Steinberg BA, Dorian P, Anstrom KJ, et al. Patient-Reported Outcomes in Atrial Fibrillation Research. JACC Clin Electrophysiology. https://doi.org/10.1016/j.jacep.2019.03.008.
9. Spertus J, Dorian P, Bubien R, et al. Development and Validation of the Atrial Fibrillation Effect on Quality –of-Life (AFEQT) Questionnaire in Patients with Atrial Fibrillation. Circ Arrhythm Electrophysiol. 2011; 4:15-25. https://doi.org10.1161/circep.110.958033.
10. Zhao DS, Shen Y, Zhang Q, et al. Outcomes of catheter ablation of atrial fibrillation in patients with hypertrophic cardiomyopathy: a systematic review and meta-analysis. Europace. 2016;18 (4):508–20.
Received: May 16, 2022
Accepted: June 27, 2022
Published: June 29, 2022.
To cite this article : Williams KM, Blatchford PJ, Laws FA. Long- Term Outcomes Following Endocardial and Epicardial Ablation of Atrial Fibrillation in a Low Procedural Volume Hospital. British Journal of Heart Diseases. 2022;4(1): 194-197. doi: 10.31488/ bjhd.118.
©2022 Williams KM, et al.