Research article/ Open Access
DOI: 10.31488 /bjhd.112
Device Motion Indication Guidance Reduces Longitudinal Geographical Miss Occurrence during Implantation of Coronary Stents
Rami Abu Fanne, Simcha Ron Meisel, Majeed Zahalka, Ariel Roguin, Yaniv Levi,Aharon Frimerman
1. Department of Cardiology, Hillel Yaffe Medical Center Affiliated with Rappaport Faculty of Medicine, Technion- Israel Institute of Technology, Haifa, Israel
*Corresponding author: Aharon Frimerman, M.D, Hillel Yaffe Medical Center, POB 169, Hadera, Israel 38100.
Abstract
Background: The cyclic movement of the heart promotes relative longitudinal movement between the coronary arteries and the pre-deployed devices potentially resulting in malpositioning. We previously introduced the device motion index (DMI) feature of the SyncVision system as an efficient tool to reliably extract this relative longitudinal movement. At that time we instantaneously adopted a new approach of stent elongation corresponding with the DMI-derived relative movement. We sought here to assess a possible contribution of this implementation to mitigating longitudinal geographical miss (LGM). Methods: We retrospectively analyzed all-comer patients who underwent SyncVision assisted stenting from March 2013 to July 2013 at our center. Two experienced interventional cardiologists independently reviewed all steps of the percutaneous coronary intervention procedures to determine the occurrence of LGM according to pre-specified criteria. Results: 193 patients underwent a DMI-guided percutaneous coronary intervention with 218 branch point sites identified. Retrospectively reviewing the angiograms we found a low incidence of longitudinal GM (2.3%). Both one-year target lesion revascularization (2.2%) and target vessel revascularization (2.8%) rates were favorable. Conclusions: Appreciating the impact of heart movement on geographical miss occurrence seems imperative. We suggest rethinking margins of effective PCI: beyond using the plus 4mm traditional margins to cover distal and proximal edges, it seems prudent to integrate the typical coronary segment displacement value in the final stent-length selection.
Keyword: geographical miss, Stent deployment, thrombosis, restenosis
Introduction
The term geographical miss was first introduced in the field of radio-oncology [1] to define a low radiation dose-induced treatment failure. This nomenclature was later adopted in interventional cardiology to define a coronary segment that was injured but received sub-therapeutic, low-dose radiotherapy [2, 3]. Currently, in the stents era, inadvertent stent deployment entirely or partially missing the target lesion is termed GM.
The STLLR (Stent deployment Techniques on cLinicaL outcomes of patients treated with the cypheRTM stent) trial was the leading study addressing GM [4]. Retrospectively judged GM was reported in 67% of the participants and was associated with significantly increased risk of target vessel revascularization (TVR) and myocardial infarction (MI).
Essentially, the coronary arteries follow the dynamic geometric changes of the heart during the cardiac cycle, as their displacement tracks that of the contiguous epicardium. These orchestrated movements led Zheng Sun et al. [5] to even advocate the extraction of myocardial dynamic information through estimating coronary arterial motion field.
The SyncVision™ System (Sync-Rx, Netanya, Israel) is an add-on image processing system with unique enhancement and stabilization power. Using the novel feature of this system, the DMI, we were previously able to delineate the typical device movement measurement (DMM) at the different coronary segments [6]. Along the entire study time our local stenting strategy was modified by adopting a SyncVision-guided DMM-driven stent elongation; we believed it might enhance full lesion coverage. In the current study we aimed to retrospectively explore a possible effect of this methodology on GM occurrence.
Methods
Patient population
We retrospectively analyzed the relevant data of one hundred and ninety-three consecutive patients who underwent percutaneous coronary intervention (PCI) with the SyncVision™ System guidance between April 2013 and July 2013. The study was approved by the local IRB at the Hillel Yaffe Medical Center, Hadera, Israel. Patients with unprotected left main disease, very tortuous coronary segments, heavily calcified and bifurcation lesions, target stenosis located in a saphenous vein or an arterial bypass graft, or life expectancy ≤12 months were basically excluded.
The DMI Feature Description
The DMI feature was described before [6]. It is an enhanced view of the vessel as seen during contrast injection (Figure 1). A 20 frames/sec angiography was utilized. Each scene was completed without any table movement. The DMM acquisition was achieved simultaneously during routine angiography, as previously described [6)]. Intra or inter-observer variability of the software was not relevant.
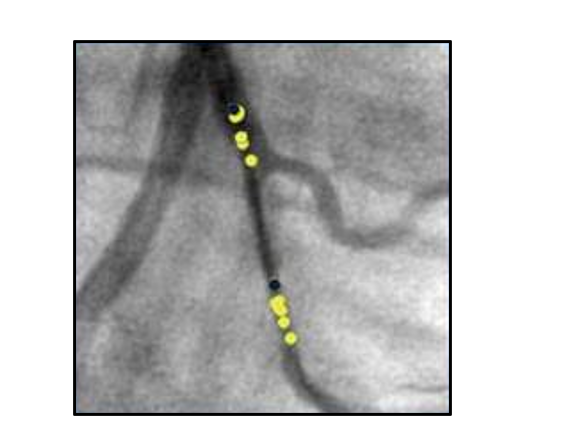
Figure 1.Illustration of the Sync-Rx-derived balloon movement in the OM artery. The yellow dots represent the cumulative locations of the balloon marker throughout the cardiac cycle. The two dark dots represent the edges of the balloon at end diastole. OM = Obtuse Marginal.
PCI methodology
Our stenting protocol at the time of our previous study was slightly modified [6]: pre-dilatation was inherently performed for plaque preparation; by default, a balloon of appropriate length was selected to cover the stenotic segment, though shorter than the planned QCA guided stent length. Assuming zero relative displacement of the balloon (DMM=0), the “traditional stent length” aimed to cover the target coronary lesion, including the entire segment injured by the balloon, plus 4 mm to better cover the proximal and distal landing zones. Virtually, the only modification in our routine stenting methodology was adding the DMM value to the final stent length to get, what we termed, the 'optimal stent length'. High pressure post-dilatation using noncompliant balloons shorter than total stent length was routinely applied. The DES implanted was Resolute Integrity (Medtronic), and the BMS used was TITAN (Hexacath).
Retrospective angiographic assessment for longitudinal GM
The angiographic procedures were retrospectively analyzed and interpreted by two independent invasive cardiologists to determine the occurrence of longitudinal GM (LGM) according to the criteria described by costa et al. [4]. The team meticulously followed all sequences of the stenting process: pre-intervention image, balloon inflations, and stent positioning in the same projection using SyncVision™ software. The boundaries of the lesion and injured and stented segments were accordingly determined and quantified. LGM was considered in case of stent uncovering balloon injury, lesion, or both. In case of inter-observer variability the angiographic procedures were assessed by a third interventional cardiologist and the two similar decisions were listed as the designation.
Endpoints at 12-month follow-up
In addition to LGM determination, the post-procedure one-year outcomes of target lesion revascularization (TLR) and TVR (including repeated PCI or bypass surgery of the target vessel) were recorded. Safety measures of MI, stent thrombosis, and death were also documented.
Statistical analysis
Statistical analysis was performed by IBM Statistics.20. Quantitative data are presented as mean ± SD. Comparison of data for statistical significance was assessed using Student's unpaired t-test. Significant differences were defined when the p value was less than 0.05 using a 2-tailed test.
Results
Using the Sync-Rx system we previously confirmed substantial device displacement on real time cineangiography [6]. Realizing that stent deployment precisely at the late diastolic phase is inapplicable, and appreciating the inevitable occurrence of stent movement prior to its implantation, we modified our stent implantation methodology translating the measured balloon movements into the practice of deploying stents of extra length.
The DMI acquisition was successful in 100% of the procedures. Two-hundred and eighteen lesions in 193 patients (1.1 ± 0.4 per patient) were stented. The admission diagnosis was troponin positive events in 64.2% and troponin negative in 35.8%. Mean age 60±11.6 years. The segments treated included ninety-eight left anterior descending (LAD) lesions (65 proximal, 25 mid and 8 diagonals), forty-nine left circumflex (LCX) lesions (14 proximal, 6 mid, 24 1st marginal and 5 2nd marginal) and seventy-one right coronary artery (RCA) lesions (30 proximal, 26 mid, 9 distal, 4 RPDA and 2 RPLA). The mean extra stent length directed by the DMM values was 3.3±0.7 mm at the RCA, 2.7±0.5 mm at the LCX and 2.0±0.35 mm at the LAD artery. Across the coronary bed extra stent length was the smallest at the mid LAD (1.6±0.3 mm) and the proximal LCX segments (2±0.4 mm). Roughly, 65% of the implanted stents were DES with the rest being BMS. The average lesion length was 17.1±4.5mm and the average stent length was 23.8±2.7mm.
Angiographic assessment for LGM
Impressively, the retrospectively judged LGM was described in five cases (2.3%): two mid and one distal RCA cases (average DMM=3.9 mm), and two cases of first and second marginal branches (average DMM=3.2 mm). All the LGM cases were classified as uncovered injured segment post balloon dilatation. No inter-observer variability was encountered.
Clinical follow up at 12 months
TVR occurred in 6 patients (2.8%). The TLR occurred in 5 patients (2.2%): two proximal LAD stents (2 proximal diagonals), 2 mid-distal RCA lesions and one distal LCX stent. The heart rate was <80 bpm and LV contractility was normal in 80% of patients. The admission diagnosis was unstable angina in 80% and elective staged PCI in 20%. Of note, 80% of TLR cases occurred in bare metal stent (BMS) treated segments at a median time of 6 months following the index intervention (range: 2.5-11 months). IVUS and/or OCT modalities for stent failure illumination were not used, as these modalities are not reimbursed at our center. Reviewing the TLR angiographic data we noticed an average DMM value of 2.8 mm; however, this was nicely covered by a long corresponding stents leaving no estimated LGM by the independent team. On the other hand, when assessing the lesions for potential axial GM we could appreciate 3 cases meeting the criteria defined by Costa (one case of proximal undersized stent and 2 cases of distal oversized stents). Concurrently, 3 out of the 5 cases were also diabetic. Safety end-points included one case with ST elevation MI (outside the target vessel). No death or stent thrombosis was reported. The five cases with estimated LGM reported no clinical events.
Discussion
We have previously described the unique pattern of the relative coronary "balloon displacement" at the different coronary segments [6]. We estimated that this displacement could be a relevant contributor to LGM unless the regular methodology of stent deployment was modified. On an ad hoc basis, we translated the concept of measurable coronary segment oscillation to the practice of utilizing extra stent length. Retrospectively tested, the average DMM-derived extra stent length at the RCA was approximately 1.21 times that of the LCX, and 1.64 times that of the LAD.
Different studies using different modalities proved LGM to be common, occurring in 30–45% of angiographically-guided PCIs, despite satisfactory and meticulous angiography guided stent positioning. Applying Costa team [4] definition of LGM we show that our easy to apply DMM based stenting nearly abolished LGM occurrence.
Retrospectively evaluating their stent implantation policy, Costa et al. found significantly increased incidence of TLR and TVR in patients judged to sustain LGM during stent deployment. Rigorous assessment of the STLLR data disclose that the average lesion and stent lengths were 16.54±10.10 mm and 18.3-19.1±6 mm, compared to 11.857±6.6 mm and 18.3±6.19 mm, in the GM and no-GM groups, respectively. In the present group the average lesion length was 17.1±4.5 mm corresponding to average stent length of 23.8±2.7 mm. Intriguingly, when calculating the difference between stent to lesion length in the study by costa et al. it is clear that the no-GM arm markedly exceeded the GM arm with 6.4 mm vs. 2.6 mm, respectively. In our group the averaged difference was 6.65 mm.
Calvert PA et al. used virtual histology IVUS prior to and after PCI and showed GM to be associated with more vulnerable plaque composition, eventually resulting in a worse prognosis [7]. In this respect, we do appreciate the role of IVUS and/or OCT in allocating hot spots/ruptured plaques in the vessel, together with optimizing stent length evaluation. Noteworthy, at the event of stent deployment the DMM concept is not incorporated into the IVUS guided strategy. We believe that optimizing radial stent apposition (ameliorating axial GM) is the main virtue of IVUS usage.
There have been several techniques suggested to reduce the cardiac-cycle related movement of the stent delivery system including holding breath, deep guiding catheter engagement, anchor wire technique, buddy wire technique, floating wire technique, rapid right ventricular pacing and rapid coronary wire pacing, the majority of which are cumbersome and impractical. Applying the relatively simple and accessible SyncVision-supported DMM derived concept, might prove beneficial in LGM control.
Conclusions
We introduce the measurable relative balloon displacement at the different coronary segments as a potential modifiable factor in the occurrence of LGM. The Sync-Rx System derived coronary segments displacement mapping should be incorporated in the final stent length; instead of using the plus 4mm traditional margins to cover distal and proximal edges we suggest adding the specific segmental values as provided in our simplified coronary segments motion map (Figure 2).
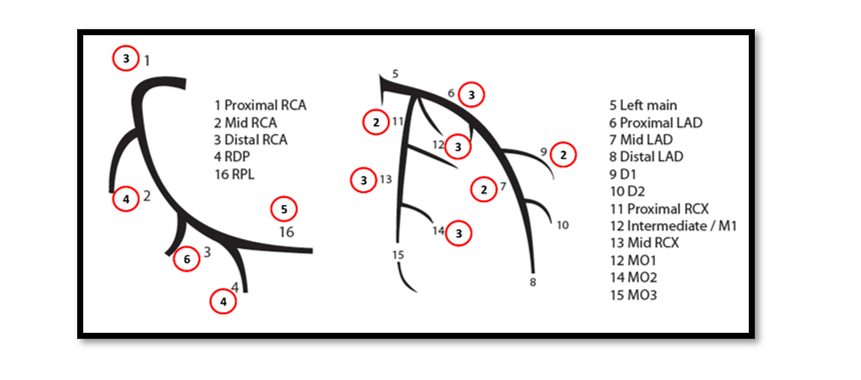
Figure 2.Simplified coronary segments motion map- coronary artery segments and each corresponding relative displacement (red circle).
Study Limitations
Our study is an observational one. A randomized trial with a control group is mandatory in order to establish the clinical relevance of our observation. Also, the study period is a little pit past; however, we focused on the same study group of our previous research [6], and included the retrospectively judged LGM with the follow up data. We do use the Sync-Rx System regularly; however the measured DMI data are not readily available. Moreover, ever since the relevant study period we are more frequently using IVUS and/or IFR/FFR in our routine PCI procedures which might potentially change our standard simplified policy at the time of the study.
We described our results pointing to the endpoints of the STLLR study. The STLLR study retrospectively analyzed the angiographic data for axial GM determination, proving null effect on MACE occurrence. Accordingly, we did not attempt to comprehensively analyze axial GM.
Abbreviations
DMI: device motion index; GM: geographical miss; PCI: percutaneous coronary intervention; TVR: target vessel revascularization; MI: myocardial infarction; DMM: device movement measurement; QCA: quantitive coronary angiography; LGM: longitudinal geographical miss; TLR: target lesion revascularization; IVUS: intravascular ultrasound.
Statement of Ethics
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. Subjects enrolled have given their written informed consent and the study protocol was approved by the local IRB at the Hillel Yaffe Medical Center, Hadera, Israel.
Conflict of Interest Statement
Prof. Aharon Frimerman is a consultant to Sync Rx, Netanya, Israel. Other authors have no competing interests to declare.
Funding Sources
No funding.
Author Contributions
Rami Abu Fanne- conception/design/acquisition and analysis of the work; drafting the work and revising it critically for important intellectual content, final approval, agreement to be accountable for all aspects of the work. Simcha Ron Meisel- analysis of the work; revising it critically for important intellectual content, final approval, agreement to be accountable for all aspects of the work. Majeed Zahalka- acquisition and analysis of the work; agreement to be accountable for all aspects of the work. Ariel Roguin- acquisition and analysis of the work; final approval, agreement to be accountable for all aspects of the work. Aharon Frimerman- conception/design and analysis of the work; revising it critically for important intellectual content, final approval, agreement to be accountable for all aspects of the work. Yaniv Levi- acquisition and analysis of the work; agreement to be accountable for all aspects of the work.
References
1. Sabaté M, Costa MA, Kozuma K. Geographic Miss: A Cause of Treatment Failure in Radio-Oncology Applied to Intracoronary Radiation Therapy. Circulation. 2000;101:2467-71.
2. Kim HS, Waksman R, Cottin Y, Kollum M, Bhargava B, Mehran R. Edge Stenosis and Geographical Miss Following Intracoronary Gamma Radiation Therapy for In-Stent Restenosis. J Am Coll Cardiol 2001;37:1026 –30.
3. G Sianos, I P Kay, M A Costa, E Regar, K Kozuma, P J de Feyter. Geographical miss during catheter-based intracoronary beta-radiation: incidence and implications in the BRIE study. Beta-Radiation In Europe. J Am Coll Cardiol. 2001;38: 415-420.
4. Marco A Costa, Dominick J Angiolillo, Mark Tannenbaum, Mitchell Driesman, Alan Chu, John Patterson, et al. Impact of Stent Deployment Procedural Factors on Long-Term Effectiveness and Safety of Sirolimus-Eluting Stents (Final Results of the Multicenter Prospective STLLR Trial). Am J Cardiol 2008;101:1704 –17.
5. Zheng Sun, Ya Zhou. Assessing Cardiac Dynamics based on X-Ray Coronary Angiograms. Journal of Multimedia. 2013;8: 48-55.
6. Rami Abu Fanne, Simcha Ron Meisel, Avraham Shotan, Aharon Frimerman. Device Motion Indication: A Novel Image-Based Tool to Measure Relative Device Motion During Coronary Intervention. J Invasive Cardiol. 2017;29:421-424.
7. Patrick A Calvert, Adam J Brown , Stephen P Hoole , Daniel R Obaid, Nick E J West , Martin R Bennett. Geographical miss is associated with vulnerable plaque and increased major adverse cardiovascular events in patients with myocardial infarction. Catheter Cardiovasc Interv. 2016;88:340-7.
Received: August 25, 2021;
Accepted: September 02, 2021;
Published: September 06, 2021.
To cite this article : Fanne RA, Meisel SR, Zahalka M, et.al. Device Motion Indication Guidance Reduces Longitudinal Geographical Miss Occurrence during Implantation of Coronary Stents British Journal of Heart Diseases. 2021; 2:1.
©2021 Fanne RA, et.al.