Research/ Open Access
DOI: 10.31488 /bjhd.115
Carotid Artery Stenting Complications – Prevention and Treatment
Marcelo José de Almeida1,2 MD, PhD, Ludvig Hafner1,2 MD, PhD, Vivian Fernanda do Amaral1 BS
1.Marilia Medical School, Department of Surgery, Marilia Medical School FAMEMA, Marília, SP, Brazil
2.Department of Vascular and Neurovascular Interventional Radiology, SIRVAN, Marília, SP, Brazil
*Corresponding author: Marcelo José de Almeida, Marilia Medical School, Department of Surgery, Marilia Medical School FAMEMA, Marília, SP, Brazil
Introduction
In the 80s, the surgery of the carotid occlusive disease began to be performed by vascular and endovascular surgeons using a new resource: catheters, balloons, and stents. The technique presented the attractive innovation of performing surgery with local anesthesia, less hospitalization, and the opportunity to preserve cerebral blood flow during the procedure, also made possible the simultaneous treatment of common and internal carotid lesions [1]. In addition, clinical surveillance during the procedure allowed early diagnosis and rescue of intracerebral thromboembolic complications.
The endovascular treatment of carotid bulb atherosclerosis disease with stent “Carotid artery Stenting” (CAS), only recently presented results similarly with endarterectomy [2]. For the endovascular treatment of carotid atherosclerosis to be an option for carotid endarterectomy, it should be considered that the surgical risk should not be greater than the risk of the natural history of the disease and results should be similar of carotid endarterectomy, consequently treatment with carotid stenting should have less than 6% of complications in symptomatic patients and less than 3% in asymptomatic patients [3].
Outcomes of CAS demonstrated different results in groups of professionals who performed this technique [4]. The improvement of materials and the surgeons experience observed in some groups to acquire skills in this type of treatment, became good results only in some groups of endovascular surgeons.
Continuous learning and the need to look "in the rearview mirror" and observe what can be improved to the technique is the objective of this chapter: to anticipate and prevent the main complications and perform early diagnosis and intervention when they occur to minimize harm to patients.
Considerations about medical staff, equipment, and materials
Endovascular treatment of the carotid artery requires training. In addition to the anatomical knowledge already acquired in the early stages of medical degree, the operator should have foundations on access to the aortic arch, the morphology of the region, the variations of the vessels of the supra-aortic trunk and the cerebral arteries. Additionally, you should have detailed knowledge about the various types of catheters you have with its wide variety of tips, introducers and guides available as well as the quality, support, and hydrophilia of the materials. The knowledge of the surgical arch and the injector pump and its available resources, the contrast to be used with the volume and pressure injected are also important elements for performing cerebral angiography followed by angioplasty and Stent implantation. The Society of Vascular Surgery (SVS) recommends performing at least 30 brain angiography and 25 carotid angioplasties, which will give, according to this society, a basic experience to the operator [4]. It is observed that this number has been established empirically, but it is important to highlight that the operator should have minimal initial experience. In view of this fact, it is suggested that the procedures performed when starting the learning curve are always performed together with a more experienced professional. Of course, the practice is continuous and will be consolidated in the patient's choice, in the improvement of surgical time, in the choice of the most appropriate material and in the advanced ability of handling the materials; these facts will become in better results of endovascular treatment of the carotid [5-7].
Patient choice
The patient's factors that may interfere with the endovascular procedure for the treatment of carotid stenosis are:
● Anatomy of the aortic arch and vessels of the supra-aortic trunk.
Calcifications, severe tortuosity, multiple plates in the catheter passage path and anatomical changes such as bovine arch may hinder the procedure [8-10].
● Severe kinking tortuosity of the internal carotid artery immediately above the bulb; may cause problems in positioning, releasing, and removing the brain protection filter [8-10].
● Atherosclerotic changes in the femoral or humeral access vessels; arteries of very narrow diameter or with stenosis are obstacles to the introduction of endovascular devices.
● Low brain reserve of the patient with presence of dementia; are predictors of poor results in CAS, in this case carotid bulb revascularization will not promote a clinical improvement that justifies the risk of the procedure [5-7].
● Intracranial study demonstrating associated diseases such as cerebral aneurysms or severe intracranial atherosclerotic involvement; in these situations, a risk-benefit of the procedure should be analyzed and the need to plan simultaneous or early treatment of intracranial brain alterations should be analyzed [11,12].
In summary some essential factors should be considered and interfere with the results in endovascular treatment, below are some of them (Table 1):
Table 1:Factors interfering with the success of carotid angioplasty and Stent implantation
| Medical team, equipment, and materials Proper team training: physicians, nurses, and |
| Proper team training: physicians, nurses, and x-ray technicians |
| Digital angiography equipment preferably in the operating room, good quality digital subtraction angiography images and technological courses with “road mapping” and measurements of arterial stenosis performed by the equipment, technically favor the procedure |
| Injector pump with safety mechanisms and alerts in case of bubbles in the injection system and pressure elevation in contrast injection |
| In the angiography room, a variety of catheters, guides and stents should be available |
| Factors related to the patient's anatomy |
| Aortic arch should not exhibit excessive tortuosity |
| Presence of thrombi in arterial walls, "shaggy aorta" increased risk |
| Check if vessels of the supra-aortic trunk present favorable angulation (Figure 1) |
| Analyze arterial access points for catheter insertion |
| Avoid the procedure in a patient with marked tortuosity of the internal carotid artery (difficulties in using the brain protection filter |
Step by step on CAS - types of complications and how to avoid them
Complications in access areas
To avoid intracranial embolization or Stent thrombosis, patients who will undergo CAS are protocolized with two platelet antiaggregant: aspirin and clopidogrel or ticagrelor, in addition, intraoperative non-fractionated heparin is used, the use of these medications alter hemostasis and increase the incidence of complications related to hematoma at puncture sites at catheter access points. The preferential access to CAS is the common femoral artery, but alternative areas such as humeral access or even the common carotid artery in the cervical region can be used [13].
The main complications in the access areas are local bleeding and hematomas in 0.5% of the cases, pseudo aneurysms, retroperitoneal hematomas, and arteriovenous fistulas, 0.15% of the cases [14,15]. To reduce complications of the arterial access point, the ultrasound study allows the operator to perform the puncture in areas of arterial wall less affected by atherosclerosis and the perforation should preferably be only in the anterior arterial wall. In addition, the use of materials with minor profile (caliber of introducers and catheters) and use of occlusions type "plugs" in the puncture area when finishing the procedure also decrease the incidence of this type of complication.
Complications caused by catheters passage in the aortic arch and arteries of the supra-aortic trunk
The passage of the catheter in the aortic arch and the selective catheterization of the common carotid artery and passage of the guiding catheter requires attention and technical care. It should be noted that the internal carotid artery has not yet received the brain protection device and thus the friction of the catheter tip in the arterial wall can cause cerebral embolisms, also contrast injection should be careful because the presence of air in the injection syringe can result in gas embolism.
Aortic arches of type 2 or 3 or very tortuous, the presence of irregularities, calcifications and thrombi of the arterial wall are elements that hinder the passage of catheters. To prevent these complications, it is necessary to perform preoperatory planning. Angiotomographic study of the arch and vessels of the supra-aortic trunk is important because it allows a prior selection of the catheters to be used and the approach pathways at lower risk [16] (Figure 1).
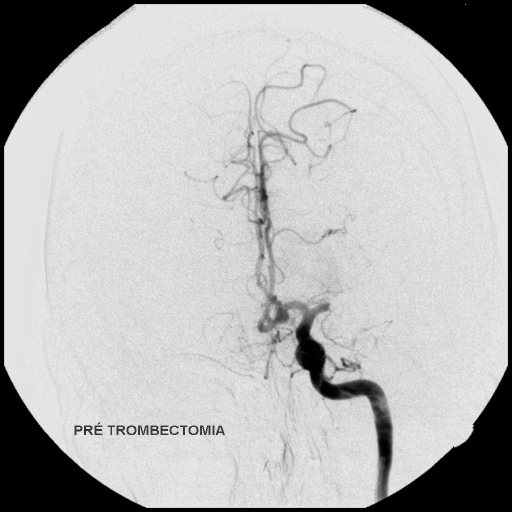
Figure 1:Types of aortic arch. The arrow indicates a greater degree of difficulty in passing catheters
For the catheterization of the common carotid artery, low-profile diagnostic catheters are recommended, with good torque and rounded tip, without edges; technically, catheter and guide should be positioned along the axial axle of the artery. This care will prevent the catheter from shaved into the arterial wall and thus prevent particles from moving into intracranial cerebral circulation.
The catheterization of the external carotid and the use of hydrophilic and support guides allow the passage of the catheter to have a coaxial guide, offering less risk. In this technique, the anchoring guide in the external carotid artery is used to support the device, as the guide catheter is positioned in the middle segment of the common carotid artery the system containing the hydrophilic support guide and the guide catheter dilator are gently removed keeping it localized 2 to 3 cm away from the carotid bulb area to be treated. After this maneuver, the contents of the guiding catheter are aspirated and, in the absence of plate or thrombi, the perfusion of the guide catheter with saline solution begins perfusion pressure just above the patient's systolic pressure throughout the procedure.
Another type of technical approach consists in positioning the catheter guide next to the ostium of the common carotid artery, simultaneously the diagnostic and guide catheter is introduced to have diagnosis and guide, and using the support coaxial system gradually the device is gently pushed until it is positioned near the carotid bulb, this is a technical option when there is occlusion of the external carotid artery and also a preferential option of hemodynamicists due to the experience of these professionals in the treatment of coronary heart disease.
Overtaking of stenotic lesion - complications caused by the passage of the brain protection filter
After positioning the guide catheter in the common carotid artery, the crossing of the stenotic lesion should be performed, it is a phase that requires increased attention because we do not yet have the cerebral protection system installed. Friction caused by the passage of the filter or guide through the plate can highlight particles to the central nervous system and cause a stroke (CVA). Plate irregularities, arterial tortuosity and very serious synthesis add an extra risk at this stage. The use of the lower profile brain protection device and those with two-step filter overtaking, first guide 0.014 and then filter, minimize the risks at this stage. The technique with amplification of the image to angioscopy and the "Road mapping" are important because they allow the visualization of the guide path in fluoroscopy and the adjacent arterial structures, thus allowing to direct the guide in the intraluminal path in order to bypass the arterial curves and the edges of the irregular plate.
Consistent studies support the need for the use of the brain protection filter, the device is associated with a lower rate of cerebral thromboembolic complications when compared to the implantation of carotid stent without the use of the filter. In view of this fact, endovascular treatment of the carotid artery is not recommended without the use of protective devices that can be filtered or by temporary occlusion of the internal carotid artery [17].
After the stenotic lesion, the cerebral protection filter should be positioned 30 mm above the plate, and in the path of the most rectilinear internal carotid artery possible. The release should be smooth and without “back-and-go” movements of the device. Arteriography should confirm the correct positioning of the filter and whether the released filter has good coaptation at the edges of the artery. The complications of CAS in this step are caused by filter implantation in tortuous arterial segments or reduced filter diameter compared to the internal carotid artery, these changes can prevent the edges of the filter from fully touching the diameter of the arterial lumen resulting in leaks through the arterial edges and particle migrations to the brain (Figure 2).
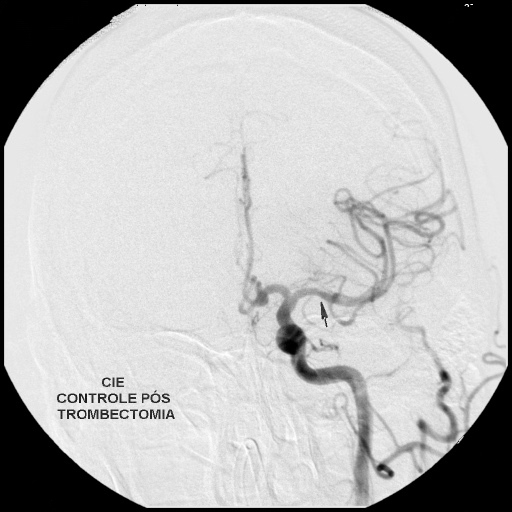
Figure 2:Position of the brain protection filter
Passage of the pre-dilation balloon – a way to avoid intracerebral embolization in the passage of the stent
The use of the pre-dilation balloon creates a space or a pathway that favors the passage of the device containing the self-expanding Stent. Attempting to pass the stent without pre-dilation can cause friction of the edges of the device on the plate to cause fragment migrations and exceed the retention capacity of the brain protection filter.
Considerations on stent positioning and release - how to avoid misplacement of the stent
Complications caused by migrations and poor stent positioning are not despicable. It is estimated that the rate of complications in this phase is around 0.25% [18]. Care in the release of the stent includes good positioning and maintenance of the release device in a linear manner with the guide; according to the types of stents we have different release devices and the careful reading of the manual must be done prior to the use of the device, the release system most used by the industry is known as "pull back" in this system, usually with the left hand of the operator, is carried out the firm and delicate locking of the distal segment of the release device, with the right hand gently performs the gentle traction of the sheath which in turn will release the stent carefully and under fluoroscopic visualization in order to deposit the stent precisely in the desired place.
Post dilation – complications caused by extrusion of the plate by the stent meshes with consequent cerebral embolization – how to avoid
The time of post dilation and stent accommodation is essential in CAS. The post dilation refers to the step in which after stent implantation an angioplasty balloon is inserted to expand the stent. At this stage the expansion of the stent can cause the extrusion of softer elements of the plate by its meshes and these atherosclerotic fragments in large amounts can eventually escape through the brain protection filter resulting in cerebral embolization or completely filling with plaque debris or thrombus the space between the stent and the brain protection filter. Complications of this type occur in 0.5% of cases [19,20].
At this time of CAS and with the objective of avoiding complications special attention should be given to the characteristics of the implanted stent and the diameter of the balloon:
Stent Features
The free spaces between the stent meshes are called stent cells. In closed cell stents all the edges of the meshes that make up the stent cell are connected, thus favoring a better coating of the plate, and are preferably indicated for ulcerated plates. This fact promotes better coverage of the arterial surface and decreases the phenomenon of plate extrusion in post-dilation; however these devices are more rigid and have difficulty in accommodating arterial tortuosity. In open cell stents only part of the edges that make up the stent cells are connected, thus having the advantage of accommodating to arterial tortuosity, however, care should be taken in the post-dilation, because the larger space of the stent cell results in greater extrusion of the plate elements with consequent greater number of embolic fragments. There are also mixed cell stents, in these the V-mesh design is constructed with greater contact area of the edges of the stent meshes, in this way this design has less cell space compared to the open cell stent being more flexible than the closed cell stent, this device aims to combine two benefits, promote better stent accommodation and lower plate extrusion. Finally, there are stents available with an external PTFE coating consisting of a 500 micros screen, these devices were built to prevent the extrusion of the plate by stent cells. Initial studies have shown good results; however, a larger sample and long-term follow-up should support the use of this material [21,22].
Balloon diameter
Regarding the choice of balloon diameter in post-dilation it is recommended that the Stent is not expanded to its nominal size. The gentle accommodation of the Stent, possibly maintaining 10 or 20% narrowing compared to its diameter, can be accomplished without compromising the result. Thus, for Stents of 8 mm in diameter the use of balloons of 5.5 mm or 6.0 mm in diametral lows the effectiveness of the treatment with lower risk of extrusion of the plate, at the same time the diameter of the vessel in the region of stenosis will reach the nominal value of the diameter of the internal carotid artery after the bulb making the treatment effective [20,23] (Figure 3,4).
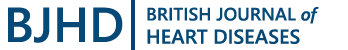
Figure 3:Pretreatment carotid angiography
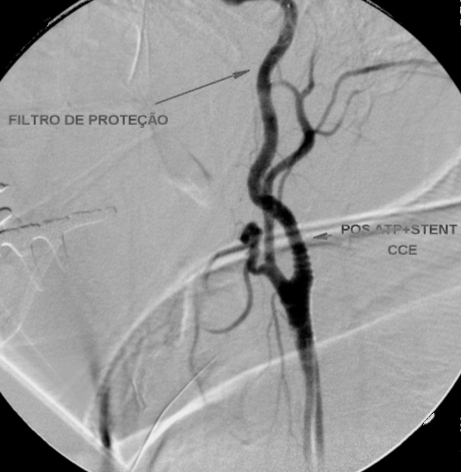
Figure 4:Post-treatment carotid angiography
Very long or excessively short stents: two problems to avoid
For treatment with stent implantation in carotid disease to have its protective effect and avoid stroke, attention should be given to the length and diameter of the stent. Short stents result in their "encrusting" in the plate, this fact causes mechanical stimulation resulting in faster plate growth and early stent occlusions. Otherwise, the uncovered edges of the plates, because they present elements of high risk of embolization can cause early complications such as stroke and stent occlusions. Excessively long Stents can also result in problems, this factor occurs preferentially in tortuous arteries; the presence of a more rigid intra-arterial element tends to keep the artery straight and lengthens the tortuous artery to its extremity, at this point there are torsions and arterial folds that can limit blood flow resulting in complications.
Thus, in addition to the characteristics of the stent, the correct dimensioning of the extension and diameter of the stent are important elements in the CAS. The stent should fully cover the plate area and the diameter should respect the nominal size of the common carotid artery immediately before the bulb, given this fact most operators experienced in the CAS recommend that the stent should be positioned in the common carotid artery near the bulb with the distal end positioned in the internal carotid artery 5 to 10 mm after the end of the compromised arterial area. For straight arteries, closed cell stents that "conform" less to the vessel but perfectly line the plate is the best option, for tortuous arteries open or mixed cell stents that will accommodate the stent inside the vessel have better results [19].
There are also conical stents, in these the proximal segment has a larger diameter to accommodate the common carotid artery and the distal segment has a smaller diameter to accommodate the internal carotid artery. There are no differences in the rate of complications between the conical stents and the retos [24].
Withdrawal of brain protection mechanisms - Watch out! It's not over yet...
The use of brain protection devices is an essential element in the treatment of carotid bulb lesions. In this way, even if steps are added in the procedure such as placing and removing the filter or temporary occlusion device, the protection device should always be used.
Just like the filter implant, the moment the protective device is removed should be taken care of to minimize complications.
The removal of protective filters is responsible for 1.1% of stroke cases in CAS [25], complications occur by:
● Difficulty in transporting the "filter releaser" by coaxial route, in these cases the excessively tortuous artery or stent meshes end up preventing access to the filter.
● Brain protection filter with large number of thrombotic elements exceeding the filter compartment and partially filling the internal carotid artery distally to the filter.
● Temporary occlusion device may cause friction in the artery with plaque detachment, or the patient may be occlusion intolerant.
In these cases, it is necessary to act prudently avoiding sudden maneuvers. To solve the first problem mentioned, it is suggested to gently climb the guiding catheter inside the stent. This movement will prevent the lifter from screwing into the stent meshes. The alignment of the devices formed by the protection filter guide, stent, and catheter guide results in a better proximal ascent of the filter releaser. If this maneuver is not effective, the filter removal can be replaced with a 125 cm 5F hydrophilic catheter, this catheter can be used as a filter removal, however this maneuver is outside the descriptive use of the product. The open filter should never be moved to the guiding catheter, as the elements contained in the filter are likely to detach ascending to the central nervous system (CNS).
In the second case, an occlusion of the internal carotid artery is usually observed on the control angiography due to many thrombi inside the filter. Removing the filter will cause the number of thrombi external to the filter to embolize into the CNS. For these cases it is suggested the use of diagnostic catheter of 125 cm, this catheter can be used in the same filter guide or parallel to this, navigating the catheter guide to the filter area. From this moment on, aspiration is performed by the catheter of the thrombotic elements that are lodged in the internal carotid artery immediately downstream of the filter. After this aspiration, the catheter is removed and a new arteriography is performed. If the thrombotic elements were adequately aspirated, arteriography will allow visualization of the internal carotid artery. The filter is then carefully removed using the withdrawal device.
The use of occlusion protection devices is responsible for complications like filter protection devices [26]. The MO.MA is formed by an axis with three lumens (one working channel and two insufflation/deflation channels) and two balloons located near the distal end of the catheter and another 6 cm proximal to this. By being inflated, respectively in the external carotid artery and common carotid artery, the balloons disrupt the ipsilateral carotid flow to the brain and generate an inverse flow into the internal carotid artery, preventing fragments originating from the atherosclerotic plate from being treated to embolize the brain. The content between the balloons and the internal carotid can be aspirated through the work door located between the two balloons. Through this same door, access to the internal carotid artery is performed for angioplasty and stent implantation. For occlusion devices of this type, the blood material present between the occlusion balloon of the common and external carotid artery should be aspirated before the flow release. The removal of the balloons should be careful to avoid damage to the arteries. Occlusion by the device should be done with the conscious patient to observe if there are no clinical signs of cerebral ischemia. Some patients do not tolerate temporary occlusion of the internal carotid artery and prevent the use of this system.
Control arteriography - avoid complications
At the end of the implant and post-stent dilation, arteriography of the carotid arteries of the cervical region and intracranial carotid artery and its branches are performed. In the Famema Medical School, FAMEMA, (member of the RHEUNI group) it is carried out in a standard way after the removal of the brain protection filter the repetition of extra and intracranial arteriography.
In the intracranial angiographic evaluation, the arterial, arteriolar, and venous phases are analyzed to identify small embolization. An objective and succinct clinical examination is also performed in which motricity, sensitivity of the limbs, speech and comprehension of some words are also performed, thus intending to identify small clinical alterations. In the RHEUNI group series of 294 patients submitted to ATP and carotid Stent, there was 1 death (0.7%) and 8 patients presented some type of cerebral ischemic event (5.7%), interesting to note that early diagnosis allowed total reversal of ischemic events in 4 patients (2.85%): in a patient reported with Broca's aphasia, analysis of intracranial arteriography identified a small filling failure in the corresponding artery, in this specific case as the artery was very delicate and the very small lesion was chosen to perform the passage of selective microcatheter and the manual injection of 15 mg of tissue plasminogen activating thrombolytic (rTPA) intra-catheter having for 15 minutes, there was complete recovery of symptoms; in 3 patients, filling failures were identified in the A1 segment of the anterior cerebral artery or in the M1 segment of the middle cerebral artery. For these cases, intracranial intervention was performed using a "Solitaire" thrombus removal device. It consists of a type of stent that is deposited on the thrombus, after a period, the small cage that is fixed to on guide wire 0.014 is removed and removes the thrombus that is trapped inside the device, this form restores intracranial circulation. In our series, 2 patients had success with complete clinical recovery and 1 patient remained with upper limb paresis. In the comparative study conducted by the RHEUNI group, when evaluating the results in 30 days of 806 patients although the rate of complications of percutaneous carotid treatment was higher than conventional surgical treatment there were no statistically significant differences. When evaluating MACCE (Major adverse cardiac and cerebral events) events in 30 days, it is also observed that the results were similar, especially if the complete recovery of 3 patients or 2.13% who had complete recovery are considered (Figure 5).
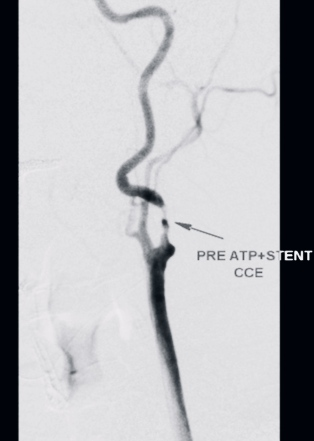
Figure 5:Occlusion of the middle cerebral artery segment M1 pos ATP
Final Considerations
Currently, world statistics indicate that the complications caused by carotid Stent implantation are similar to open surgical treatment. The possibility of opting for a procedure according to the characteristics of age, anatomy, and anesthetic risk are opportunities for choice for the surgical team in the indication of treatment of carotid atherosclerosis. It is necessary, in a similar way to endarterectomy, observe a technical discipline for performing the CAS that will determine the success of the procedure. There are two elements in the percutaneous treatment of the carotid that should be observed: the diagnosis of intracranial alterations is early and accurate and allows immediate treatment and rescue of complications in most patients.
References
1. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Endarterectomy for asymptomatic carotid artery stenosis. JAMA. 1995; 273: 1421-1428.
2. CAVATAS Investigators. Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): a randomized trial. Lancet. 2001; 357: 1729-1737.
3. Goldstein LB, Adams R, Alberts MJ, et al. American Heart Association/American Stroke Association Stroke Council; Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group. Stroke. 2006; 37: 1583-1633; 2006.
4. Barr JD, Connors JJ, Sacks D, et al. Quality improvement guidelines for the performance of cervical carotid angioplasty and stent placement. J Vasc Interv Radiol. 2003;14: S321-S335.
5. Chiam PT, Roubin GS, Iyer SS, et al. Carotid artery stenting in elderly patients: importance of case selection. Catheter Cardiovasc Interven. 2008; 72 (3): 318-324.
6. Roubin GS, Iyer S, Halkin A, et al. Realizing the potential of carotid artery stenting: proposed paradigms for patient selection and procedural technique. Circulation. 2006; 113 (16): 2021-2030.
7. Sayeed S, Stanziale SF, Wholey MH, et al. Angiographic lesion characteristics can predict adverse outcomes after carotid artery stenting. J Vasc Surg. 2008; 47: 81-87.
8. Macdonald S, Lee R, Williams R, et al. Delphi Carotid Stenting Consensus Panel: Towards safer carotid artery stenting: a scoring system for anatomic suitabilitt. Stroke. 2009; 40 (5): 1698-1703.
9. Vogel TR, Dombrovskiy VY, Haser PB, et al. Carotid artery stenting: impact of practitioner specialty and volume on outcomes and resource utilization. J Vasc Surg. 2009; 49(5): 1166-1171.
10. Barr JD, Connors JJ, Sacks D, et al. Quality improvement guidelines for the performance of cervical carotid angioplasty and stent placement. J Vasc Interv Radiol. 2003;14: S321-S335.
11. Hofmann R, Niessner A, Kypta A, et al. Risk score for peri-interventional complications of carotid artery stenting. Stroke. 2006; 37: 2557-2561.
12. Chiam PT, Roubin GS, Panagopoulos G, et al.: One-year clinical outcomes, midterm survival, and predictors of mortality after carotid stenting in elderly patients. Circulation. 2009; 119 (17): 2343-2348.
13. Ates M, Sahin S, Konuralp C, et al. Evaluation of risk factors associated with femoral pseudoaneurysms after cardiac catheterization. J. Vasc Surg. 2006; 43: 520-524.
14. Messina LM, Brothers TE, Wakefield TW, et al. Clinical characteristics and surgical management of vascular complications in patients undergoing cardiac catheterization: interventional versus diagnostic procedures. J Vasc Surg. 1991; 13: 593-600.
15. Ricci MA, Trevisani GT, Pilcher DB. Vascular complications of cardiac catheterization. Am J Surg. 1994;44, 1205-1211; 1994.
16. Verzini F, Cao P, De Rango P, et al. Appropriateness of learning curve for carotid artery stenting: an analysis of periprocedural complications. J Vasc Surg. 2006; 44: 1205-1211.
17. Kastrup A, Groschel K, Krapf H, et al. Early outcome of carotid angioplasty and stenting with and without cerebral protection devices: a systematic review of the literature. Stroke. 2003; 34: 813-819.
18. Okasaki T, Sakamoto S, Shinagawa K, et al. Detection of in-stent protrusion (ISP) by intravascular ultrasound during carotid stenting: Usefulness of stent-in-stent placement for ISP. Eur Radiol. 2018.
19. Fanous AA, Jowdy PK, Morr S, et al. Vascular Anatomy and Not Age is Responsible for Increased Risk Symptomatic Elderly Patients Undergoing Carotid Artery Stenting. World Neurosurgery. 2019; https://doi.org?10.1016/ World Neurosurg, 04.187; 2019.
20. Millet JD, Cavallo JJ, Scoutt LM, et al. Sonographic Evaluation of Complications of Extracranial Carotid Artery Interventions. J Ultrasound Med. 2017. https://doi:10.1002/Jum.14376
21. Kotsugi M, Takayama K, Myouchin K, et al. Carotid Artery Stenting Investigation of Plaque Protusion Incidence and Prognosis. JACC: Cardiovascular Intervention. 2017; 10: 824-831.
22. Schneider PA, Levy E, JM Bacharach, et al. A First-in-Human Evaluation of a Novel Mesh-Covered Stent for treatment of Carotid Stenosis in Patients at High Risk for Endarterectomy. 30-day Results of the Scaffold Trial. JACC: Cardiovascular Interventions. 2018; 11: 23.
23. Gruber P, Berberat J, Kahles T, et al. Comparison of different carotid stent designs in endovascular therapy of servere carotid artery stenosis. Clin Translacional Neurosci. 2020.
24. Boisiers M, Deloose K, Verbist J, et al. What Practical Factors Guide the Choice of Stent and Protection Device during Carotid Angioplasty. Europ J Vasc Endovascular Surg. 2008; 35 :637-643.
25. Reimers B, Schluter M, Castriota F, et al. Routine use of cerebral protection during carotid artery stenting: results of a multicenter registry of 753 patients. Am J Med. 2004; 116: 217-222.
26. Tatli E, Buturak A, Grunduz Y, et al. Comparison of anti-embolic protection with proximal ballon occlusion and filter devices during carotid artery stenting: clinical and procedural outcomes. Postepy Kardiol Interwencyjnej. 2013; 9 (3): 221-227.
Received: February 07, 2022;
Accepted: February 28, 2022;
Published: March 03, 2022.
To cite this article : de Almeida MJ, Hafner L, do Amaral VF. Carotid Artery Stenting Complications – Prevention and Treatment. British Journal of Heart Diseases. 2022;4(1): 175-181. doi: 10.31488/bjhd.115.
©2022 de Almeida MJ, et al.